Introduction
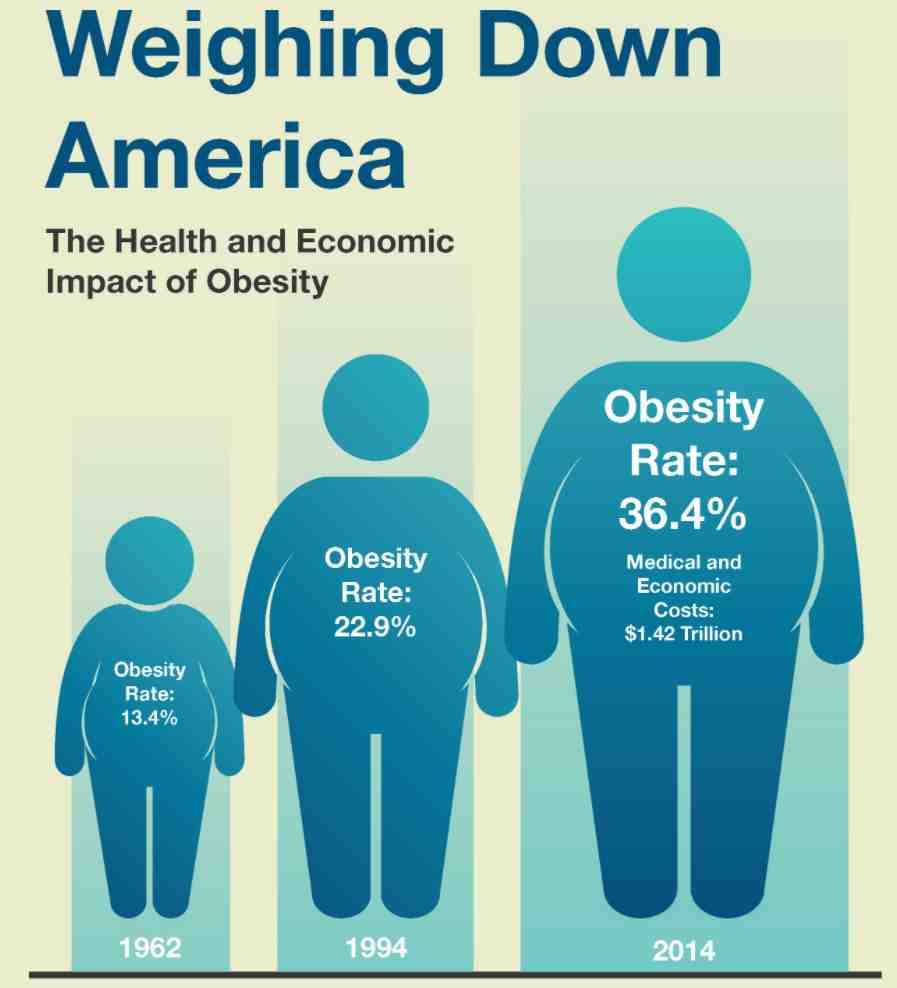
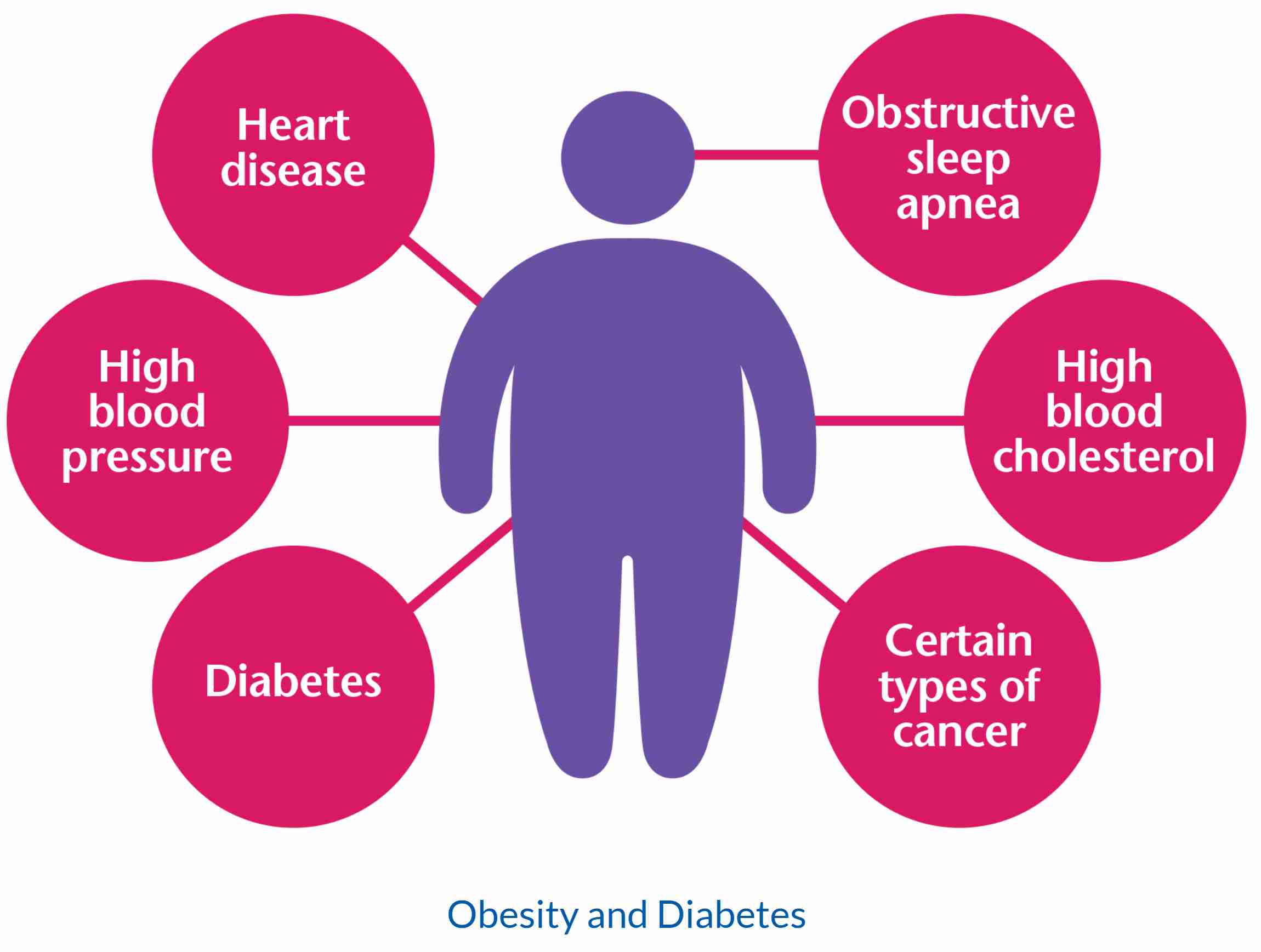
Obesity is a major risk factor for many non-communicable diseases which can be developed as a result of obesity (Ofei, 2007). Obesity is a global epidemic that affects all age groups. Social and lifestyle changes have been attributed to the rising cases of obesity across the world, especially in developed countries. Together with being overweight, obesity comprises over a third of the worlds’ population (Hruby & Hu, 2015). The consumption of junk foods that are rich in fat and carbohydrates has led to the increased chances of obesity (Ash et al., 2017). To add on, reduced physical activity has attributed to the rising trend. Consequently, international, as well as community based campaigns have been launched to encourage people to maintain healthy body weights in order to prevent or manage existing conditions of obesity (Ash et al., 2017). The campaign aims at emphasising the need for the reduction of excessive food consumption and eating a healthy balanced diet to control obesity based complications.
Moreover, the campaign also encourages individuals to increase the amount of physical activities that they do, which burn fat and thus would lead to the reducing of chances of having the conditions of obesity (Schaap et al., 2018). In some cases, body-weight reduction pills and techniques have been used to reduce obesity. Some of the interventional practices recommended have seemed to be quite detrimental to people’s health, and thus raises ethical, social, and health concerns.
The Data Collection Methods
The research that was conducted used secondary sources of data based on their availability, cost effectiveness, and reliability. The study conducted extensive research on scientific literature that has previously been done, they include contents from books, journals, and magazines to clearly understand the reliability of the widely held opinion that obesity is caused by the lack of or insufficient physical exercises and a poor diet. In addition, the research relied on online sources from nutritional advisers and medical care organisations that have done extensive research on the topic. Similarly, it used primary information sources by conducting a survey and using a questionnaire to gather personal opinions from a randomly selected sample.
Behaviour Change Theory
Historically, preventative measures of obesity focused on the behaviour adjustment theoretical framework to understand the causative agents of weight gain. Additionally, they focused on physical activities and healthy eating practices that help reduce weight (Stice et al., 2019). Despite the compelling nature of this aspect, the diversity and complexity of the issue are of great concern (Peterson, 2018). According to Gibbs et al. (2011), basing the management of obesity on behavioural theories sounds ridiculous and naïve and insensitive to ethical issues and the economic perspective.
More convincing theories pin the issue on the biological and genetic features of an individual (Suglia et al., 2016). Gender and age of an individual also play a vital role (Gibbs et al., 2011). Moreover, theories on social ecology are gaining acceptance in explaining how the eating habits, physical activities, and weight gain of individuals are affected by social and environmental factors (Dochat et al., 2020). Thus, a better understanding of socio-environmental theories can enable comprehension of the element that contributes to society, and therefore, looking for solutions to the pandemic will be easy.
The Aim of the Campaign and the Outcome Variable
There are several community based interventions that have been taken to control the rising cases of obesity with some of these interventions being based on a single community, while others are targeted on a specified geographical zone that is deemed to have a high number of reported cases of obesity (Blake-Lamb et al., 2016). These interventions are considered to encourage residents of the targeted community to have a lifestyle change by reducing activities that increase the chance of becoming obese and promote those that reduce the probability of getting the condition.
The Methodology of the Campaign
Most of the notable campaign strategies include the hiring of sports trainers, providing playgrounds, mobilising people to participate in the Olympics, and sponsoring games to increase physical activities of an individual, especially in youths (Peterson, 2018). In schools and other institutions, the campaign is aimed at encouraging fruit and vegetable consumption. Therefore, a notable introduction of these commodities has been noted. The campaign is also targeted at identifying obese family members as well as children to offer counsel on weight reduction strategies and also encourage them to see a health professional.
The Target Population
Most of the community based interventions address the whole community by focusing on the activities of the entire population rather than concentrating on the affected group. This target population of the whole community is a desirable progression because, over the past years, weight gain is observed in all groups of people and not only in the obese community (Blake-Lamb et al., 2016). If the trend is not controlled, then the likelihood of numerous reported cases will become a critical phenomenon (Ward et al., 2017). Most of the community based campaigns have focused on encouraging behavioural changes that promote a controlled body weight through physical activities and healthy eating. Nevertheless, since body gain is not only attributed to eating and physical activities but also stress, sleepless nights, and other health co-morbidities, the campaigns also address them too.
The Selected Risk Factor
Obesity is a lifestyle condition that is caused by several factors. Primarily, the consumption of junk food that is rich in sugar has been predisposing an individual to get obese. Besides, reduced physical activity can increase the probability of being obese. Similarly, particular diseases such as diabetes increase the chance of an individual from being obese.
An individual who develops obesity experiences both psychological and physical torture. They become emotionally overwhelmed as they struggle to meet the societal demands of moderate body weight. Notwithstanding, the body can experience joint pain as a result of heavy weights that can need medical attention. Treating this condition is associated with financial constraints as well as painful struggles that leave the patient emotionally drained.

A Critique of the Health Campaign
Research has questioned the various interventions recommended by the campaign to address the obesity issue in the community (Simpson, Griffin and Mazzeo, 2019). For instance, there is enough evidence to support the claim that the recommended interventions have effectively addressed the obesity issue among community members. Furthermore, several researches have established that the results of these interventions are not long-lasting in reducing or maintaining body weight. The published results of several campaigns indicate that children are more likely to benefit from the change in physical activities as well as diet as they are generally more quick to adjust to a new program than the adults (Baker et al., 2017). To add on, campaigns that explicitly focused on weight loss indicated poor outcomes (Palmeira et al., 2017).
Similarly, the benefits of maintaining the recommended body weight have always been overstated and amplified by media and other platform outcomes (Palmeira et al., 2017). The emphasised benefit has overshadowed physical and psychological toll likely to be subjected to those involved in the campaign. The physical exercises and changes in diet rarely focus on the morphological variation that exists amongst participants based on their age, ethnicity, and body structures (Escandón-Nagel et al., 2018). The already established perception of the positivity of maintaining a healthy body weight may be detrimental to some people, especially those with an underlying medical condition (Baker et al., 2017).
Despite the positive results of physical exercises, evidence has emerged that most of the obese people undergoing practical classes have experienced physical and psychological abuse. Some have reported being mistreated by their trainers by subjecting them to strenuous physical activities that result in injuries or excessive fatigue (Escandón-Nagel et al., 2018). Society expects that all people should maintain a healthy weight, therefore putting undue pressure on overweight people, such as fat women. When an excessively overweight person drastically loses weight, they develop undesirable physical characteristics, such as wrinkles, stretch marks, and sagging skin that can pose mental distress to the individual.
In case dietary change and physical activities do not result in a reduction of body weights, doctors may recommend weight reducing pills and, in some cases, perform surgery. Some of the recommended medications hinder or alter some physiological processes in the body resulting in weight loss. However, according to (Dochat et al. 2020), the intended result is not always specific since most of them only achieve less than five percent weight-loss despite their adverse health complications. Drugs have been unable to offer a long-lasting solution since their effects are notable over a short period, after which the patient may return to their original body form. Even though surgery has shown remarkable achievements, the procedure is quite expensive, thus limiting the number of patients who can undergo the procedure (Ward et al., 2017). Moreover, the procedure might become complicated and a patient may get severe complications that can lead to death if not appropriately managed.
The Success and the Potential Success of the Campaign
The campaign to encourage people to reduce their weight has a significant impact on society. According to Jones et al. (2017), members of society are aware that it is essential to maintain a healthy body weight to minimise cases of obesity. Awareness of the importance of doing physical activities no matter how trivial it might look has contributed significantly in the society. If the campaign incorporates the shortcomings expressed by this paper, it is likely to achieve significant results toward achieving an obesity free society. Those who develop and become overweight will be encouraged to participate in activities that can minimise their weight rather than the current stigma that they face. In addition, if the campaign can focus on preventative measures, fewer people would develop obesity which would save on costs of treatment and management practices. Furthermore, the pain and suffering associated with weight reducing techniques would be evaded if people do not develop obesity.
Conclusion
Health campaigns on obesity which are poorly supported by existing evidence have the potential to harm some patients. A diversified intervention strategy is needed to address the situation and solve the issue in a myriad of ways to incorporate genetic and environmental factors that are generally ignored yet contribute significantly to the rising number of obesity cases around the world. Policy makers should make regulations that encourage healthy eating and physical activities so that obesity can be reduced. Incentives should be provided to those willing and those who show effort to live healthy lives. The food industry and hospitality organisations should promote healthy eating by incorporating a menu that increases the consumption of a balanced diet that is likely to minimise the chances of leading people to obesity.
References
Ash, T., Agaronov, A., Aftosmes-Tobio, A., & Davison, K. K. (2017). Family-based childhood obesity prevention interventions: a systematic review and quantitative content analysis. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 113.
Blake-Lamb, T. L., Locks, L. M., Perkins, M. E., Baidal, J. A. W., Cheng, E. R., & Taveras, E. M. (2016). Interventions for childhood obesity in the first 1,000 days a systematic review. American journal of preventive Medicine, 50(6), 780-789.
Baker, P., Gill, T., Friel, S., Carey, G., & Kay, A. (2017). Generating political priority for regulatory interventions targeting obesity prevention: an Australian case study. Social science &Medicine, 177, 141-149.
Dochat, C., Afari, N., Wooldridge, J. S., Herbert, M. S., Gasperi, M., & Lillis, J. (2020). Confirmatory factor analysis of the Acceptance and Action Questionnaire for Weight-Related Difficulties-Revised (AAQW-R) in a United States sample of adults with overweight and obesity. Journal of Contextual Behavioral Science, 15, 189-196.
Escandón-Nagel, N., Peró, M., Grau, A., Soriano, J., & Feixas, G. (2018). Emotional eating and cognitive conflicts as predictors of binge eating disorder in patients with obesity. International Journal of Clinical and Health Psychology, 18(1), 52-59.
Jones, J., Yoong, S. L., Wyse, R., Ward, D. S., & Wolfenden, L. (2017). Improving the impact of obesity prevention interventions in the childcare setting: The need for a systematic application of implementation science. Journal of paediatrics and child health, 53(3), 211-213.
Ofei, F. (2007). Obesity – A preventable disease. Ghana Medical Journal, 39(3), 98.
Palmeira, L., Pinto-Gouveia, J., Cunha, M., & Carvalho, S. (2017). Finding the link between internalized weight-stigma and binge eating behaviours in Portuguese adult women with overweight and obesity: The mediator role of self-criticism and self-reassurance. Eating behaviors, 26, 50-54.
Peterson, R. (2018). Fed Up with the Personal Responsibility Narrative of Obesity: A Pentadic Analysis. Kentucky Journal of Communication, 37(2).
Schaap, R., Bessems, K., Otten, R., Kremers, S., & van Nassau, F. (2018). Measuring implementation fidelity of school-based obesity prevention programmes: a systematic review. International Journal of Behavioural Nutrition and Physical Activity, 15(1), 75.
Simpson, C. C., Griffin, B. J., & Mazzeo, S. E. (2019). Psychological and behavioural effects of obesity prevention campaigns. Journal of health psychology, 24(9), 1268-1281.
Stice, E., Desjardins, C. D., Shaw, H., & Rohde, P. (2019). Moderators of two dual eating disorder and obesity prevention programs. Behaviour research and therapy, 118, 77-86.
Suglia, S. F., Shelton, R. C., Hsiao, A., Wang, Y. C., Rundle, A., & Link, B. G. (2016). Why the neighbourhood social environment is critical in obesity prevention. Journal of Urban Health, 93(1), 206-212.
Ward, D. S., Welker, E., Choate, A., Henderson, K. E., Lott, M., Tovar, A., … & Sallis, J. F. (2017). Strength of obesity prevention interventions in early care and education settings: a systematic review—preventive Medicine, 95, S37-S52.


